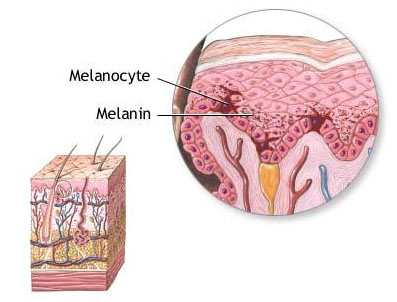
The melanocytes form and store the colour-giving skin pigment melanin in the melanosomes (cell organelles). They are located in the stratum basale of the epidermis and in the hair follicle, where they provide the individual colouring. The degree of melanin formation determines the skin type. A melanocyte forms a unit with approx. 36 keratinocytes. Keratinocytes are the predominant cell type of the epidermis. [1]
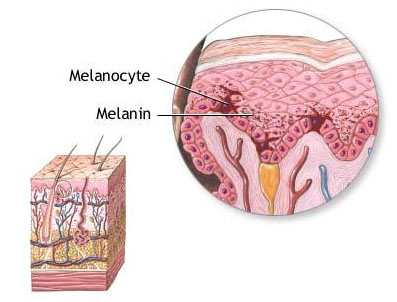
Fig. 1: Melanocyte in the skin [6]
Melanogenesis
When the skin is irradiated with UV light, the melanin is transported in front of (supranuclear) the cell nucleus of the keratinocytes in the direction of the radiation incidence. The DNA in the cell nucleus of the keratinocytes is thus protected from genetic damage. The resulting tanning of the skin is the externally visible sign of cell protection. [1]
Pigmentation disorders
Locally increased amounts of stored melanin lead to limited hyperpigmentation. Conversely, hypopigmentation is produced by changes in melanocyte density and deficits in melanin synthesis or melanosome function. [2]
Postinflammatory hyperpigmentation
Unlike pigmentation triggered by UV radiation, post-inflammatory hyperpigmentation (PIH) is a reaction of melanocytes to endogenous influences, such as inflammatory acne. Exogenous inflammations, e.g. caused by burns, also trigger PIH regardless of the skin type. The intensity of PIH increases with the activity of the melanocytes. [3]
The melanocytes react to damage to the dermo-epidermal junction zone (connecting zone between the epidermis and dermis) by increasing melanin production and the transport of the skin pigment. [2] In the process, the pigment is either stored in the keratinocytes or released directly into the dermis. [4]
Mechanisms of PIH formation in the dermis
Three mechanisms are discussed in the literature:
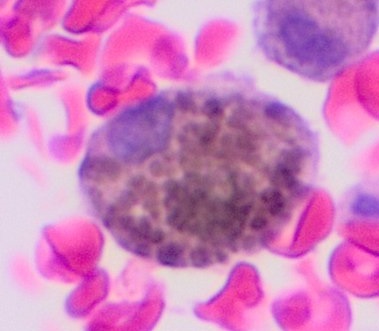
- During the inflammatory process, the melanocytes in the stratum basale are destroyed. The melanin contained is released into the dermis and absorbed there by macrophages (scavenger cells), forming melanophages. The hyperpigmentation becomes visible on the skin from the outside.
- Melanin empties directly from the melanosomes into the dermis via dendritic connections and thus becomes visible externally.
- Macrophages migrate into the epidermis, phagocytose the melanosomes and then return to the dermis as melanophages and discolour the skin by accumulating there. [4]
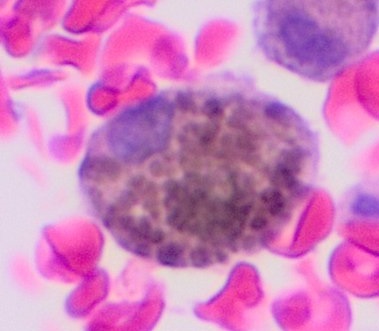
Fig. 2: Microscopic image of a melanophage [7]
External appearance
PIH is usually limited to the area of skin affected by inflammation. UV radiation can intensify the pigmentation. [5] Pigment accumulations in the epidermis produce brown to dark brown efflorescences that regress on their own after a few months. Pigment in the dermis appears dark brown and sometimes blue-greyish. The dermal pigment deposits decrease more slowly or they remain permanently. [3] The intensity of the hyperpigmentation correlates with the activity of the melanocytes (see above), but not with the preceding degree of inflammation. [5]
Treatments
The treatment of PIH in dermatology is carried out preparatively and/or device-assisted. With the help of corticoids, retinoids, hydroquinone, azelaic acid and also peelings, the pigmentation is lightened. It should be noted that irritation can occur again due to the concentration. However, pigmentation of the dermis does not respond well to preparative treatments.
On the device side, pigment accumulations in the dermis can be removed with lasers. Lasers can also trigger irritation and produce a new PIH. [5] Liposomal serums containing ascorbyl phosphate (vitamin C phosphate), applied both before and after laser treatment, can reliably prevent re-pigmentation.
Literature
- I. Moll, Dermatologie, Georg Thieme Verlag, Stuttgart 2005, ISBN 978-3131266866
- O. Braun-Falco et. al., Dermatologie und Venerologie, Springer Medizin Verlag, Heidelberg 2005, ISBN 978-3540405252
- B. P. Kaufman et. al., Am J Clin Dermatol 2018, 19 (4), 489-503
- R. Ruiz-Maldonado, M. de la Luz Orozco-Covarrubias, Seminars in Cutaneous Medicine and Surgery 1997, 16 (1), 36-43
- C. E. Orfanos, C. Garbe, Therapie der Hautkrankheiten, Springer-Verlag, Berlin Heidelberg 1995, ISBN 978-3540584124
- Unknown Author, Public domain, via Wikimedia Commons
- Mikael Häggström MD, Public Domain, via Wikimedia Commons
Anne Schieferecke |