When we talk about pigment spots, what do we actually mean? In colloquial language, we understand it to mean all kinds of spots that are characterised by their different colouring from the surrounding skin. In detail, however, we are talking about various biochemical processes that result in the formation or non-formation of substances that are deposited, accumulate or even deplete in various layers of the epidermis.
A closer look at the processes reveals that they are based on a variety of physical, biochemical, chemical and microbiological triggers. If you know them, you can respond to them with specific preventive or curative treatments.
However, a general difficulty with regard to the treatments is that, despite numerous scientific studies and publications, very little is known about the discrete chemical structures of the substances formed and we still have to rely on imprecise descriptions in this respect.
Even in the case of the most intensively studied melanin, knowledge is limited to approximate structures. This makes the development of targeted treatments with appropriate active substances extremely difficult and clearly directs the focus towards prevention.
Physical triggers – UV light
Exposure to UV light results in individual stronger pigmentation on the forehead, nose and ears ("sun terraces"), as well as locally varying skin conditions, keratoses and in the form of freckles, for example, but also visible hypopigmentation, for example on low-melanin scars or skin partially affected by vitiligo. UV light initiates the stimulation of tyrosinase in the melanocytes of the basal layer and causes the amino acid tyrosine to be converted into the dark brown eumelanin via L-dopa, dopaquinone and 5,6-indolequinone with the absorption of oxygen.
The sulphur-containing amino acid cysteine is involved in the similar formation of phaeomelanin. Both together are referred to as "melanin", stored in the melanosomes and transported from the melanocytes into the corneocytes.
The fragment of eumelanin shown in Figure 1 gives an idea of the structure of melanin. It clearly shows that well penetrating and low molecular weight reducing agents such as liposomal ascorbyl phosphate ("vitamin C"), kojic acid and hydrogen peroxide can lead to visible bleaching of hyperpigmentation. They do this by reducing quinoid groupings and disrupting the extended π-electron systems that are responsible for the colouring. The reddish sulphur-containing phaeomelanin is more resistant to external agents.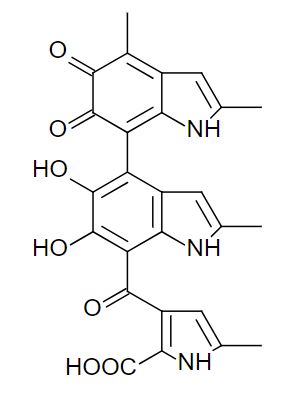
Fig. 1: Fragment of eumelanin
Otherwise, experience has shown that hyperpigmentation and freckles slowly fade by themselves if there is no further exposure to radiation or appropriate protection through clothing and sun filters.
Endogenous melanin formation
Similar to the brown colouration that occurs when an apple is injured, the epidermis is also induced to produce melanin when injured. In both cases, it is a tyrosinase that is responsible for the onset of pigmentation. It has become known as post-inflammatory hyperpigmentation, or PIH for short, and occurs after insect bites, pressure sores, urticaria pigmentosa1, chemical burns, acne and infections such as chickenpox and measles. As already mentioned, polymeric melanin structures are formed which, however, still cannot be uniformly defined chemically in detail. Hyperpigmentation also occurs during laser treatments. They can usually be completely suppressed by pre- and post-treatment with liposomal ascorbyl phosphate.
Photosensitisation is a combination of physical, chemical and endogenous melanin formation. In this case, the skin reacts particularly intensively to an orally or topically applied medication if it is followed by exposure to radiation. Contact allergens from plants, such as meadow hogweed, have the same effect. Ultimately, this is also a case of post-inflammatory hyperpigmentation.
Biochemical pigmentation
Pigment spots with a completely different composition occur on older skin, which is why they are commonly referred to as age spots. They are often associated with kidney disease or diabetes, to name just two examples.
In the English literature they are called Advanced Glycation End-Products or AGE for short. It has long been assumed that they are insoluble, poorly degradable conglomerates of proteins and sugars, similar to those formed during the reaction of self-tanning agents of the dihydroxyacetone (DHA) type with the keratin of the skin in the presence of atmospheric oxygen. From a chemical point of view, the formation of AGEs is a variant of the Maillard reaction, which starts with condensates of glucose and amino acids (Figure 2), for example, and ends with so-called melanoid structures as in the application of self-tanning agents.
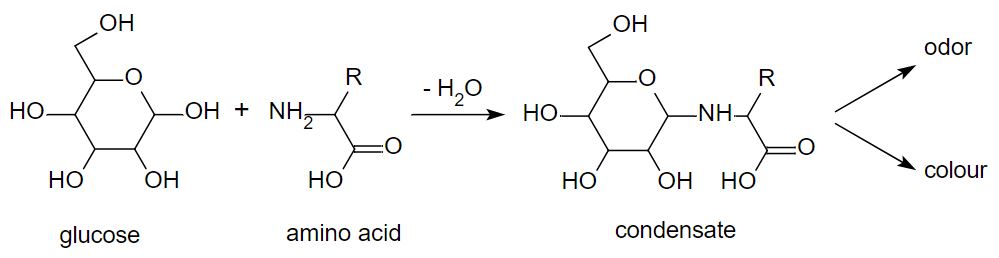
Fig. 2: Initial step of a Maillard reaction (example)
Unlike melanin pigments, AGEs do not fade seasonally and are only accessible to external treatment to a limited extent. This also applies to chemical agents. Only low-concentration hydrogen peroxide appears to have a certain effect on these polymeric condensation products. Laser treatments are usually used to remove the troublesome spots. Peels and microdermabrasion can be helpful.
Similar structures and dark colourations occur alongside odorous substances when foods containing protein and saccharides are heated during frying and baking (Figure 2).
Lipofuscin
A similar parallel with food can be drawn with pigmentation that forms from proteins or their amino acids and lipids or their degradation products. The brown colouring on the outside when frying minced meat is mainly the result of condensation reactions of proteins with fatty substances. Similar high-molecular and also very persistent compounds formed in the skin are called lipofuscin and, like AGEs, are categorised as age spots. Lipofuscin is not only found in the skin, but also in organs such as the heart, liver and kidneys. Studies have reported high molecular weight aggregates of around 6000-7000 Daltons.2
Studies on the structure of lipofuscin vary widely. Some speak of oxidised fatty acids for the lipid components, others of terpenoid isoprene structures, which are typical for retinoids. Figure 3 shows an example of a low-molecular retinoid structure.
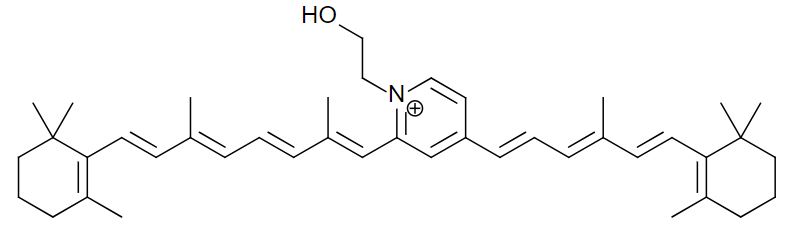
Fig. 3: Lipofuscin – example of a low-molecular retinoid structure
The different chemical compositions correspond to the varying colours of the pigmentation. They range from rather yellowish to dark brown shades. The percentages given for individual components should be treated with caution, as older information has continued to be disseminated but has not been reproduced. Accordingly, it is difficult to predict promising treatments for lipofuscin stains. In some cases, some effect can be seen with well penetrating agents such as hydrogen peroxide, which can both reduce and oxidise. However, as with AGE pigmentation, physical methods of removal are generally preferred if the skin areas in question allow.
Effectiveness measurements
The explanations about the different nature of pigment spots show a fundamental problem in finding specific cosmetic active ingredients to remove them. According to our own research, it is not possible for the service laboratories that carry out efficacy measurements to differentiate between the individual compositions of the pigments in the tests. As a result, it is not possible to categorise them and, particularly in the case of AGE and lipofuscin, there are only assumptions as to which substances could have an effect. Analysing other endogenous pigment anomalies is easier:
- Pityriasis versicolor is a superficial infection with Malassezia yeast fungi. The infected skin appears lighter in colour under daylight due to the comparatively lower melanin production. The spots appear darker on very light-coloured skin. Treatment is carried out with antimycotics.
- Pityriasis alba is a post-inflammatory hypopigmentation, i.e. areas of skin are poorer in melanin than the surrounding area. Cosmetically, it is treated with non-irritant base creams or balancing, non-occlusive foundations.
- Cutaneous mastocytosis refers to reddish-brown pigment spots that can be associated with swelling and redness. Mast cell infiltration can be detected in the dermis; in urticaria pigmentosa, the entire body is affected.
- In vitiligo, the catalase activity and the hydrogen peroxide balance of the skin are disturbed, among other things. This leads to oxidative or nitrosative (involvement of peroxinitrite) stress. Manganese salts (Mn2+) plus narrow-band UVB therapy (311 nm) can neutralise the inhibition of melanin formation. The effect of manganese corresponds to a "pseudo" catalase, which can also be observed in the form of spontaneous decomposition with the development of oxygen when manganese dioxide is sprinkled into hydrogen peroxide.
There are also many different names for the same conditions, particularly in medical terminology. For example, hyperpigmentation is also called melasma or chloasma or age spots of different composition are referred to as lentigo or lentigines (plural) with different adjectives.
Medical treatment
Typical bleaching agents are topical benzoyl peroxide (acts similar to hydrogen peroxide) and hydroquinone (tyrosinase inhibition and direct bleaching through reduction). Tretinoin (vitamin A acid) and isotretinoin stimulate the formation of new cells, while hydrocortisone reduces the pigmentation of melanocytes.
An almost similar but more moderate effect to vitamin A acid can be achieved with biodegradable cosmetic vitamin A nanodispersions.
Tranexamic acid, which is used as an antifibrinolytic (plasmin inhibitor) in medicine, inhibits the melanin formation process. It also leads to the fading of translucent blood vessels and can also be used in cosmetics in compliance with upper dosage limits. In combination with niacinamide (INCI), it is possible to intervene in melanosome transport.
Medical acid peels are still carried out with trichloroacetic acid, possibly in combination with other substances. In cosmetics, fruit acid peelings were historically developed due to the ban on vitamin A acid.
Literature
1) Yasushi Tomita, Kazuhisa Maeda, Hachiro Tagami, Mechanisms for Hyperpigmentation in Postinflammatory Pigmentation, Urticaria pigmentosa and Sunburn, Dermatologica (1989) 179 (Suppl. 1): 49–53
2) Robert D Jolly, David N Palmer, Rosalind R Dalefield, The analytical approach to the nature of lipofuscin (age pigment), Archives of Gerontology and Geriatrics Volume 34, Issue 3, May–June 2002, Pages 205-217
Dr Hans Lautenschläger |

